What is it?
- Melanoma is a type of cancer that develops in the cells that produce melanin — the pigment that gives your skin its color. Your eyes also have melanin-producing cells and can develop melanoma. Eye melanoma is also called ocular melanoma.
- Most eye melanomas form in the part of the eye you can't see when looking in a mirror. This makes eye melanoma difficult to detect. In addition, eye melanoma typically doesn't cause early signs or symptoms.
- Treatment is available for eye melanomas. Treatments for some small eye melanomas may not interfere with your vision. However, treatment for large eye melanomas typically causes some vision loss.
Symptoms
Eye melanoma may not cause signs and symptoms. When they do occur, signs and symptoms of eye melanoma can include:
- A growing dark spot on the iris
- A sensation of flashing lights
- A change in the shape of the dark circle (pupil) at the center of your eye
- Poor or blurry vision in one eye
- Loss of vision in the affected eye
Causes
It's not clear what causes eye melanoma, also called ocular melanoma. Doctors know that eye melanoma occurs when errors develop in the DNA of healthy eye cells. The DNA errors tell the cells to grow and multiply out of control, so the mutated cells go on living when they would normally die. The mutated cells accumulate in the eye and form an eye melanoma.
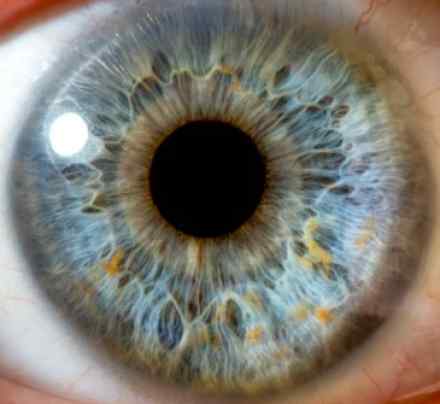
Where eye melanoma occurs
Eye melanoma most commonly develops in the cells of the uvea, the vascular layer of your eye sandwiched between the retina, the thin layer of tissue that lines the back inner wall of your eyeball, and the white of your eye (sclera). Eye melanoma can occur in the front part of the uvea (iris and ciliary body) or in the back part of the uvea (choroid layer).
Eye melanoma can also occur on the most outer layer on the front of the eye (conjunctiva), in the socket that surrounds the eyeball and on the eyelid, though these types of eye melanoma are very rare.
Risk factors
Risk factors for primary melanoma of the eye include:
- Light eye color. People with blue eyes or green eyes have a greater risk of melanoma of the eye.
- Being white. White people have a greater risk of eye melanoma than do people of other races.
- Increasing age. The risk of eye melanoma increases with age.
- Certain inherited skin disorders. A condition called dysplastic nevus syndrome, which causes abnormal moles, may also increase your risk of developing melanoma on your skin and in your eye. In addition, people with abnormal skin pigmentation involving the eyelids and adjacent tissues and increased pigmentation on their uvea — known as oculodermal melanocytosis — also have an increased risk of developing eye melanoma.
- Sun exposure. Some research suggests that people who repeatedly spend long hours in the sun may have an increased risk of eye melanoma compared with those who limit their sun exposure. But some studies haven't found a link between sun exposure and eye melanoma.
Complications
Complications of eye melanoma may include:
- Increasing pressure within the eye (glaucoma). A growing eye melanoma may cause glaucoma. Signs and symptoms of glaucoma may include eye pain and redness, as well as blurry vision.
- Vision loss. Large eye melanomas often cause vision loss in the affected eye and can cause complications, such as retinal detachment, that also cause vision loss. Small eye melanomas can cause some vision loss if they occur in critical parts of the eye. You may have difficulty seeing in the center of your vision or on the side. Very advanced eye melanomas can cause complete vision loss.
- Eye melanoma that spreads beyond the eye. Eye melanoma can spread outside of the eye and to distant areas of the body, including the liver, lungs and bones.
Diagnosis
To diagnose eye melanoma, your doctor may recommend:
- Eye exam. Your doctor will examine the outside of your eye, looking for enlarged blood vessels that can indicate a tumor inside your eye. Then, with the help of instruments, your doctor will look inside your eye. One method, called ophthalmoscopy, uses lenses and a bright light mounted on your doctor's forehead — a bit like a miner's lamp. Another method, called slit-lamp biomicroscopy, uses a microscope that produces an intense beam or line of light to illuminate the interior of your eye.
- Eye ultrasound. An eye ultrasound uses high-frequency sound waves from a hand-held, wand-like apparatus called a transducer to produce images of your eye. The transducer is placed on the eyelid or the front surface of your eye. Your doctor uses ultrasound to measure the thickness and extent of the tumor to help determine the most appropriate treatment.
- Imaging of the blood vessels in and around your eye (angiogram). During an angiogram of your eye, a colored dye is injected into a vein in your arm. The dye travels to the blood vessels in your eye. A camera with special filters to detect the dye takes flash pictures every few seconds for several minutes.
- Removing a sample of suspicious tissue for testing. In some cases, your doctor may recommend a procedure to remove a sample of tissue (biopsy) from your eye. To remove the sample, a long, thin needle is inserted into your eye and used to extract suspicious tissue. The tissue is tested in a laboratory to determine whether it contains eye melanoma cells. Eye biopsy isn't usually necessary to diagnose eye melanoma.
Determining whether cancer has spread
Your doctor may also recommend additional tests and procedures to determine whether the melanoma has spread (metastasized) to other parts of your body. Tests may include:
- Blood tests to measure liver function
- Chest X-ray
- Computerized tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Abdominal ultrasound
Treatments and drugs
Your eye melanoma treatment options will depend on the location and size of the eye melanoma, as well as your overall health and your preferences.
Waiting to treat small eye melanomas
A small eye melanoma that affects the colored portion of the eye (iris) may not require immediate treatment. If the melanoma is small and isn't growing, you and your doctor may choose to wait and watch for signs of growth. If the melanoma grows or causes complications, you may choose to undergo treatment at that time.
Surgery
Operations used to treat eye melanoma include procedures to remove part of the eye or a procedure to remove the entire eye. Options may include:
- Iridectomy. This procedure removes only a part of the iris. It's used for small iris melanomas that have not invaded other structures of your eye.
- Iridotrabeculectomy. This procedure removes parts of the iris and the supporting tissues around the cornea at the base of the iris for small iris melanomas that have invaded those tissues.
- Iridocyclectomy. This is another treatment for small melanomas of the iris and ciliary body. It involves removing part of the iris and the ciliary body.
- Choroidectomy. Part of the choroid is removed during this surgery, with or without removing part of the wall of the eye (sclerouvectomy). This complicated procedure may be followed by supplementary radiation.
- Surgery to remove the entire eye (enucleation). Enucleation is often used for large eye tumors. It may also be used if the tumor is causing eye pain. After the eye with melanoma is removed, an implant is inserted into the same position, and the muscles controlling movement of the eye are attached to the implant, which allows the implant to move. After you've had some time to heal, an artificial eye (prosthesis) is made. The front surface of your new eye will be custom painted to match your existing eye.
Radiation therapy
Radiation therapy uses high-powered energy beams, such as protons or gamma rays, to kill cancer cells. Radiation therapy is typically used for small to medium-sized eye melanomas.
The radiation is usually delivered to the tumor by placing a radioactive plaque on your eye, directly over the tumor in a procedure called brachytherapy. The plaque is held in place with temporary stitches. The plaque looks similar to a bottle cap and contains several radioactive seeds. The plaque remains in place for four to five days before it's removed.
The radiation can also come from a machine that directs the radioactive particles to your eye (external beam radiation or teletherapy). This type of radiation therapy is often administered over several days.
Laser treatment
Treatment that uses a laser to kill the melanoma cells may be an option in certain situations, but this treatment isn't widely used. One type of laser treatment, called thermotherapy, uses an infrared laser and is sometimes used in combination with radiation therapy.
Cold treatments
Extreme cold (cryotherapy) may be used to destroy melanoma cells in some small eye melanomas, but this treatment isn't commonly used.
Coping and support
Coping with vision changes
If your cancer treatment causes total loss of vision in one eye, such as happens when an eye is removed, it's still possible to do most things you were able to do with two working eyes. But it may take a few months to adjust to your new vision.
Having only one eye affects your ability to judge distance. And it may be more difficult to be aware of things around you, especially things occurring on the side without vision.
Ask your doctor for a referral to a support group or an occupational therapist, who can help devise strategies for coping and adjusting to your altered vision.
References:
https://www.nlm.nih.gov/medlineplus/ency/article/001022.htm
https://www.macmillan.org.uk/information-and-support/eye-cancer-ocular-melanoma
https://www.eyecancer.com/conditions/3/choroidal-melanoma
http://www.cancer.org/cancer/eyecancer/detailedguide/eye-cancer-survival-rates
http://www.healthline.com/health/melanoma-of-the-eye