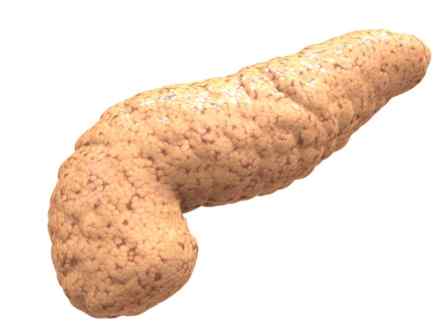
What is it?
Pancreatic cysts are abnormal, sac-like pockets of fluid on or within your pancreas. Though it may be alarming to learn you have a pancreatic cyst, the good news is that most pancreatic cysts aren't cancerous — and many don't even cause symptoms.
In fact, many pancreatic cysts aren't technically cysts at all. Called pseudocysts, these pockets of fluids aren't lined with the type of cells found in true cysts. Instead, a pseudocyst's walls may include cells normally found in other organs, such as the stomach, intestines and the pancreas itself. Pseudocysts are never cancerous.
Your doctor may want to take a sample of the pancreatic cyst fluid to determine whether it's malignant or benign. If your cyst is or can become cancerous, treatment involves surgical removal.
Symptoms
You may have pancreatic cysts, including pseudocysts, but experience no symptoms. When signs or symptoms do occur, they typically include:
- Persistent abdominal pain, which may radiate to your back
- A mass you can feel in your upper abdomen, where your pancreas is located
- Nausea and vomiting
Causes
In many cases, the cause of a particular pancreatic cyst is unknown. Some cysts are associated with rare illnesses — such as von Hippel-Lindau disease, which is a genetic disorder that can affect the brain, retina, adrenal glands, kidneys and pancreas.
Pseudocysts often follow a bout of pancreatitis, a painful condition in which the pancreas's digestive enzymes become prematurely active and digest some of the pancreas itself. Pseudocysts can also result from blunt trauma to the abdomen, such as during a car accident.
Risk factors
Heavy alcohol use and gallstones are risk factors for pancreatitis, and pancreatitis is a risk factor for pseudocysts — the most common type of pancreatic cyst.
Diagnosis
Pancreatic cysts are diagnosed more often now than in the past, but not because more people have them. Instead, improved imaging technology has made pancreatic cysts easier to find. In fact, many pancreatic cysts are found during abdominal scans for other problems.
Most pancreatic cysts can be detected by ultrasound, computerized tomography (CT) or magnetic resonance imaging (MRI) scans. Your doctor may also order an endoscopic ultrasound to visualize the cyst and to obtain fluid from the cyst for analysis. In this study, a thin flexible tube (endoscope) is passed through your mouth and into your stomach and upper small intestine. The endoscope is equipped with a small ultrasound probe to image the cyst and with a needle to obtain fluid from the cyst.
Although the majority of pancreatic cysts are benign pseudocysts, doctors may suspect another type of cyst if it occurs with no previous history of pancreatitis or abdominal injury or if it has internal walls.
In some cases, the location of the cyst in your pancreas — along with your age and sex — can help doctors pinpoint what type of cyst you have.
- Mucinous cystadenoma. These cysts are usually located in the body or tail of the pancreas and occur most often in middle-aged women. They are precancerous, and some may already be cancerous when discovered. Larger cysts are more likely to be cancerous.
- Mucinous duct ectasia. More common in men, these cysts consist of dilated ductal segments, usually within the head of the pancreas. Also known as intraductal papillary mucinous neoplasms, these growths are often cancerous.
- Serous cystadenoma. These growths can become large enough to displace nearby organs, causing such symptoms as abdominal pain and a feeling of fullness. They occur most frequently in middle-aged women and become cancerous only rarely.
- Papillary cystic tumour. The least common of the nonpseudocysts, papillary cystic tumors — also known as papillary cystic neoplasm or solid and pseudopapillary neoplasm — occur most often in young women and are usually located in the body or tail of the pancreas. They are usually cancerous.
Islet cell tumours, also known as neuroendocrine tumours, are less common. Normally, the pancreas's islet cells produce insulin and other hormones. Islet cell tumours can also produce these hormones.
References
http://www.medicinenet.com/pancreatic_cysts/article.htm
https://www.mskcc.org/cancer-care/types/pancreatic-cysts/treatment
https://www.hse.ie/eng/health/az/P/Pancreatitis,-chronic/
http://www.mayoclinic.org/diseases-conditions/pancreatic-cysts/basics/definition/con-20024331

