What is it?
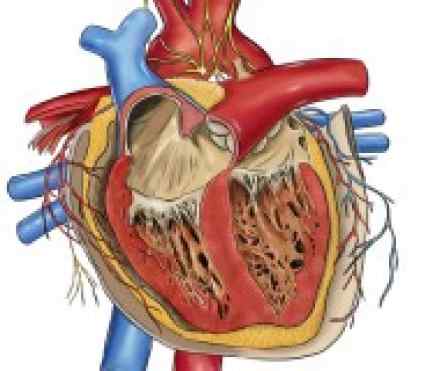
Pericarditis is a swelling and irritation of the pericardium, the thin sac-like membrane that surrounds your heart. Pericarditis often causes chest pain and sometimes other symptoms. Pericarditis is usually sudden and short-lived (acute). When symptoms develop more gradually or persist, the condition is considered chronic. The sharp chest pain associated with pericarditis occurs when the inflamed or irritated two layers of the pericardium rub against each other.
Mild cases may improve on their own. Treatment for more-severe cases may include medications and, rarely, surgery. Early diagnosis and treatment may help to reduce the risk of long-term complications.
Symptoms
Acute pericarditis usually lasts less than a few weeks. Chronic pericarditis lasts six months or longer.
If you have acute pericarditis, the most common symptom is sharp, stabbing chest pain behind the breastbone or in the left side of your chest. However, some people with acute pericarditis describe their chest pain as dull, achy or pressure-like instead, and of varying intensity.
The pain of acute pericarditis may travel into your left shoulder and neck. It often intensifies when you lie down or inhale deeply. Coughing, taking a deep breath or swallowing food also may make the pain worse. Sitting up and leaning forward can often ease the pain. At times, it may be difficult to distinguish pericardial pain from the pain that occurs with a heart attack.
Chronic pericarditis is usually associated with an accumulation of excess fluid around the heart (pericardial effusion). Often painless, the most common symptom of chronic pericarditis is shortness of breath.
Depending on the type, signs and symptoms of pericarditis may include some or all of the following:
- Sharp, piercing chest pain over the center or left side of your chest
- Shortness of breath when reclining
- Low-grade fever
- An overall sense of weakness, fatigue or feeling sick
- Dry cough
- Abdominal or leg swelling
Causes
Under normal circumstances, the two-layered pericardial sac that surrounds your heart contains a small amount of lubricating fluid. In pericarditis, the sac becomes inflamed and the resulting friction from the inflamed sac leads to chest pain.
In some cases the amount of fluid contained in the pericardial sac may increase, causing pericardial effusion.
The cause of pericarditis is often hard to determine. In most cases doctors are either unable to determine a cause (idiopathic) or suspect a viral infection.
Pericarditis can also develop shortly after a major heart attack, due to the irritation of the underlying damaged heart muscle. In addition, a delayed form of pericarditis may occur weeks after a heart attack or heart surgery because of antibody formation. This delayed pericarditis is known as Dressler's syndrome. Many experts believe Dressler's syndrome is due to an autoimmune response, a mistaken inflammatory response by the body to its own tissues - in this case, the heart and pericardium.
Other causes of pericarditis include:
- Systemic inflammatory disorders. These may include lupus and rheumatoid arthritis.
- Trauma. Injury to your heart or chest may occur as a result of a motor vehicle or other accident.
- Other health disorders. These may include kidney failure, AIDS, tuberculosis and cancer.
- Certain medications. Some medications can cause pericarditis, although this is unusual.
Complications
Complications may include:
- Constrictive pericarditis. Some people with pericarditis, particularly those with long-term inflammation and chronic recurrences, can develop permanent thickening, scarring and contracture of the pericardium. In these people, the pericardium loses much of its elasticity and resembles a rigid case that's tight around the heart, which keeps the heart from working properly. This condition is called constrictive pericarditis and often leads to severe swelling of the legs and abdomen, as well as shortness of breath.
- Cardiac tamponade. When too much fluid collects in the pericardium, a dangerous condition called cardiac tamponade can develop. Excess fluid puts pressure on the heart and doesn't allow it to fill properly. That means less blood leaves the heart, which causes a dramatic drop in blood pressure. If left untreated, cardiac tamponade can be fatal.
Early diagnosis and treatment of pericarditis usually reduces the risk of the long-term complications
Diagnosis
Your doctor likely will start by taking your medical history and asking questions about your chest pain and other symptoms. As part of your initial evaluation, your doctor will also perform a thorough physical exam and check your heart sounds.
While listening to your heart, your doctor will place a stethoscope on your chest to check for the sounds characteristic of pericarditis, which are made when the pericardial layers rub against each other. This characteristic noise is called a pericardial rub.
Your doctor may have you undergo tests that can help determine whether you've had a heart attack, whether fluid has collected in the pericardial sac, or whether there are signs of inflammation. Your doctor may use blood tests to determine if a bacterial or other type of infection is present. You may also undergo one or more of the following diagnostic procedures:
- Electrocardiogram (ECG). In this test, patches with wires (electrodes) are attached to your skin to measure the electrical impulses given off by your heart. Impulses are recorded as waves displayed on a monitor or printed on paper. Certain ECG results may indicate pericarditis, while others could indicate a heart attack.
- Chest X-ray. With an X-ray of your chest, your doctor can study the size and shape of your heart. Images of your heart may show an enlarged heart if excess fluid has accumulated in the pericardium.
- Echocardiogram. This test uses high-frequency sound waves to create a picture of your heart and its structures, including fluid accumulation in the pericardium. Your doctor can view and analyze this image on a monitor.
- Computerized tomography (CT). This X-ray technique can produce more-detailed images of your heart and the pericardium than can conventional X-ray studies. CT scanning may also be performed to exclude other causes of acute chest pain, such as a blood clot in a lung artery (pulmonary embolus) or a tear in your aorta (aortic dissection).
- Magnetic resonance imaging (MRI). This technique uses a magnetic field and radio waves to create cross-sectional images of your heart that can reveal thickening or other changes in the pericardium.
References
https://www.hse.ie/eng/health/az/P/Pericarditis/Treating-pericarditis.html
http://www.medicinenet.com/pericarditis/article.htm
http://www.heart.org/HEARTORG/Conditions/More/What-is-Pericarditis_UCM_444931_Article.jsp#.V1mckldeD1s
http://my.clevelandclinic.org/services/heart/disorders/pericarditis

